What might be the treatments available as more after-effects of Covid are discovered?
Key Takeaways
- Research led by The University of Queensland has found Covid-19 activates the same inflammatory response in the brain as Parkinson’s disease
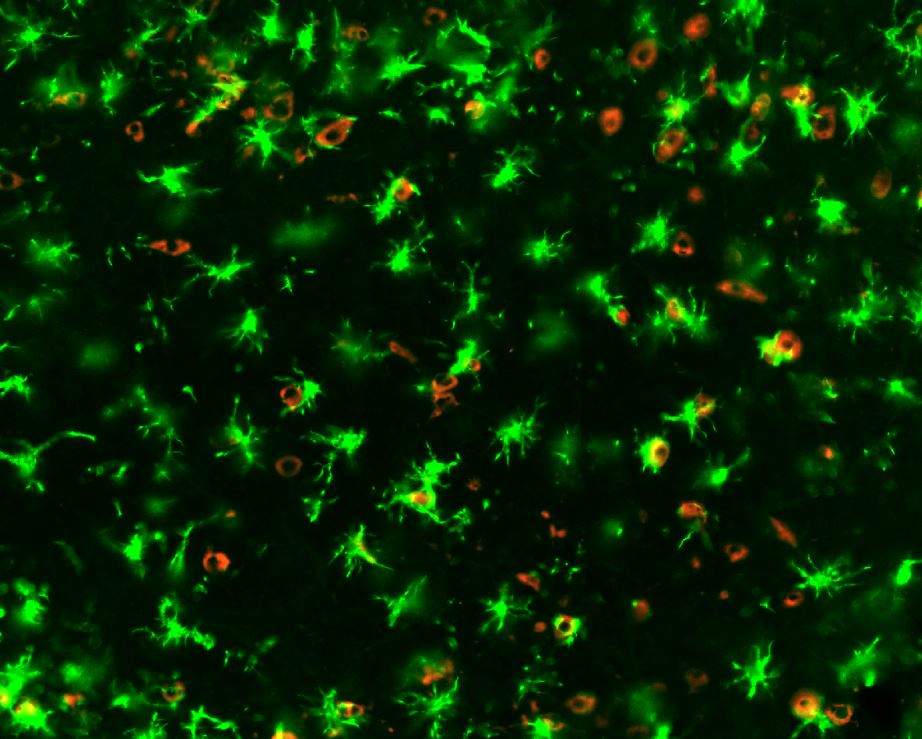
- The team was able to use human blood to enable them to study brain cells to investigate how the inflammation was creating a “fire in the brain”
- Researchers globally believe that in the coming decades, there could be a big wave of coming dementias and Parkinson’s disease
The far-reaching implications of the effects that Covid might have on the world’s population are still to be discovered.
Research led by The University of Queensland has found Covid-19 activates the same inflammatory response in the brain as Parkinson’s disease.
The discovery identified a potential future risk for neurodegenerative conditions in people who’ve had Covid-19, but also a possible treatment.
The global death toll from Covid has been more than could have perhaps been predicted, but long-term, is Covid worse than we could have ever imagined?
UQ team lead researchers Professor Trent Woodruff and Dr Eduardo Albornoz Balmaceda help Forbes Australia to gain some perspective:
Professor Trent Woodruff: “If you look back at the Spanish flu, referring to the brain, we know 20 years after there was a spike in some of these neuro degenerative disease cases. It is not unusual for these viruses to reciprocate chronically some of the things that we are referring to. There are going to be multiple consequences of these pandemics.”
Dr Eduardo Albornoz Balmaceda: “We were checking all the factors that might contribute to this chronic inflammatory process that we think is causing the neural loss for the long-term. Normally, we need to check post-mortem to see what has happened with the brain, but when we started working with the viruses, it was more about whether the virus can trigger this inflammatory processes in the brain.
The team was able to use human blood to enable them to study brain cells to investigate how the inflammation was creating a “fire in the brain”, which begins a chronic and sustained process of killing off neurons.
Dr Eduardo Albornoz Balmaceda: “It’s kind of a silent killer, because you don’t see any outward symptoms for many years. It may explain why some people who’ve had Covid-19 are more vulnerable to developing neurological symptoms similar to Parkinson’s disease.
“What we think is that someone who might have the pre-condition, that they might not know they have and can take a long time to present clinical conditions, perhaps might present with Parkinson’s disease-like symptoms after the infection with Covid. We don’t think that Covid is triggering Parkinson’s disease but somehow it could be contributing, in some individuals, to the process of accelerating the inflammation.”
Professor Trent Woodruff: “Our findings are very robust and certainly cause for more research. The good news is that we have good clinical drugs for this pathway with trials underway in Parkinson’s patients. These drugs have a long way to go through the necessary clinical steps to approval, but in theory, with their availability then that would be a potential application for patients viewed as having a higher risk of developing this post-Covid.
“The disease will march on, all patients on these therapies have already lost 60% to 70% of their neurons. We want to get to a point where we can identify patients earlier to help to prevent further neuronal loss. Looking at this inflammation, we think that is an early driver of the loss of these neurons.
“We know that the virus does have effects on the brain. It is probably transient, but it could just be one of these risk factors that may increase the risk of Parkinson’s. We think it is worth keeping an eye on. The global population is ageing, and age is the biggest risk factor for the prevalence of brain disease. There could be lots of factors, but it is definitely something that we are looking at. In the coming decades, there could be a big wave of coming dementias and Parkinson’s.”
Dr Eduardo Albornoz Balmaceda: “We’ll keep working on the long-term impacts. We’ll keep studying the brain to understand what is happening and how to use the drugs we are developing to stop the impact of perhaps long-Covid. This is not going to develop a massive wave of neurodegenerative disease, but we have some strong evidence that the virus is triggering inflammation in the brain.”
The study is published in Nature’s Molecular Psychiatry.